The male and female reproductive system are controlled by hormones released from the hypothalamus and anterior pituitary as well as hormones from reproductive tissues and organs. The hypothalamus produces Gonadotropin-releasing hormone (GnRH). GnRH stimulates the anterior pituitary gland to produce follicle-stimulating hormone (FSH) and luteinizing hormone (LH).
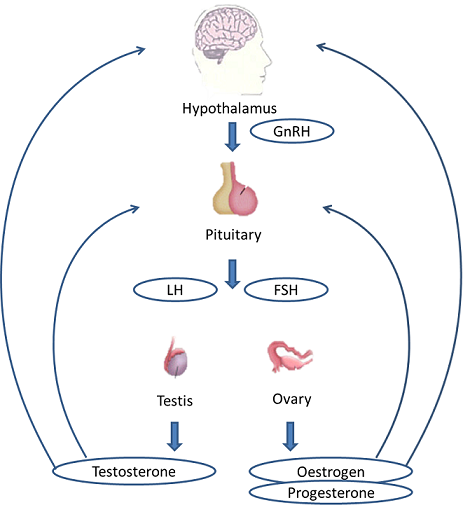
In the male, FSH and LH stimulate Sertoli cells and interstitial cells of Leydig in the testes to facilitate sperm production. The Leydig cells produce testosterone which is responsible for the secondary sexual characteristics of males.
In females, FSH and LH cause estrogen and progesterone to be produced. They regulate the female reproductive system which is divided into the ovarian cycle and the menstrual cycle. Menopause occurs when the ovaries lose their sensitivity to FSH and LH and the female reproductive cycle stops.
At fertilization, the chromosomes in one male gamete, called a sperm (or spermatozoon), combine with the chromosomes in one female gamete. Each gamete carries 23 chromosomes. Hence oocytes contain 46 chromosomes. Oocytes then multiply inside the uterus by many folds to form human life forms.
Male reproductive system
The function of the male reproductive system is to produce sperm and transfer them to the female reproductive tract. The testes are a crucial component in this process, as they produce both sperm and androgens (the hormones that support male reproductive physiology). In humans, the most important male androgen is testosterone. Several accessory organs and ducts aid the process of transport of the sperm and other seminal components to the penis, which then delivers to the female reproductive tract.
Semen and sperm
Semen is the milky fluid that a man’s penis releases during orgasm. Semen consists of fluid and sperm. The fluid comes from the prostate gland, the seminal vesicle, and other sex glands. The sperm is produced in the testicles. The seminal fluid, or semen, helps the sperm to survive in the female reproductive tract and travel towards the egg.
Any deviation from normal anatomy and physiology of male reproductive systems like hormonal imbalance, production of sperm, or abnormality in delivery systems can contribute to infertility.
Female reproductive system
For understanding female reproductive system, first we need to understand the fertilization process and menstrual cycle:
Fertilization process
Every month, a series of hormonal changes occur in the female body that causes the immature egg-containing follicle in the ovary to mature and release egg. After releasing from the ovary, the egg travels to the fallopian tube. If sperms (fertilizing cells from male partners) are present at this time in the fallopian tube, the egg can get fertilized. From the fallopian tube, the fertilized egg travels to the uterus and gets implanted in the uterine wall.
Menstrual cycle
It is the cyclical changes that occur in the female reproductive tract due to rise and fall in the level of estrogen hormone. Menstrual cycles in every woman can be of variable duration. This process takes about four weeks on average, beginning with a woman’s menstrual period.
There are 4 phases of the menstrual cycle
Menstrual phase: 1 to 5 days
The menstrual phase starts with the start of menstrual bleeding. The bleeding phase lasts for 1-5 days. Menstruation is the elimination of the thickened lining of the uterus (endometrium) from the body through the vagina.
Follicular phase : 1-16 days
The follicular phase starts on the first day of menstruation and ends with ovulation. At the starting of the cycle, follicular stimulating hormones are released (FSH) from the pituitary gland. FSH stimulates ovaries to make small sacs called follicles. These follicles contain immature eggs. The healthiest egg will mature and release from the ovary.
Ovulation phase: 14th day
The time when the egg is mature and released from the follicular sac of the ovary is known as ovulation. Rest of the follicular sac is now called corpus luteum. The released egg then travels down the fallopian tube toward the uterus. The egg is only viable for about 24 hours once it’s been released.
Luteal phase: 15th to 28th day
It is the last part of your menstrual cycle and tends to be the longest. If the egg gets fertilized the corpus luteum plays its part by maintaining progesterone levels which in turn maintains the viable environment for fertilized egg inside the uterus. If the egg is not fertilized, the corpus luteum will shrink, causing a decrease in estrogen and progesterone levels. The low hormone level will cause the uterus to shed off the endometrium and start the menstruation phase again.
Related links:

Pingback: INFERTILITY AND STRESS MANAGEMENT - by Shivhare’s Clinic
Pingback: INFERTILITY AND STRESS -
Pingback: INFERTILITY AND STRESS - Shivhare homoeopathy clinic